Benefits Buzz
You may have thought the penalty for applicable large employers who fail to offer minimum essential coverage was $2,000 per employee. You may have also thought that if you offered coverage, but it was unaffordable and/or didn’t provide minimum value, then the penalty was $3,000 per employee who waived coverage and received a subsidy in the Exchange.
- Enroll in Part B for the first time in 2016; or
- Those who don’t currently receive Social Security benefits; or
- People who have Medicare and Medicaid, and Medicaid pays the Part B premium; or
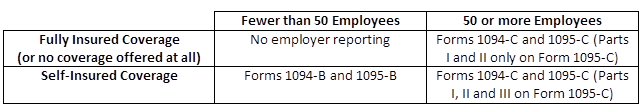
The new reporting requirements that some employers will be subject to starting next year, as required by the Affordable Care Act (ACA), will be used to help the Internal Revenue Service (IRS) enforce the Individual and Employer Mandates, and it will also help the IRS administer subsidy eligibility in the Exchanges.
The following reporting forms will be the responsibility of the employer to complete:
PCORI Fees
The Protecting Affordable Coverage for Employees (PACE) Act, signed into law by President Obama on October 7, 2015 gives states the ability to continue to determine the size of their small group market rather than conforming to a national standard.
Most states currently define their small group market as employers with up to 50 employees, but the Affordable Care Act (ACA) was set to expand that definition in 2016 to include employers with up to 100 employees. The PACE Act allows each state to independently decide what small group market definition makes the most sense.
The 2016 Medicare Part D annual enrollment period will begin on October 15, 2015 and run through December 7, 2015. Medicare beneficiaries can enroll in a Part D drug plan or make changes to existing coverage during this time period. Enrollment can be done through a stand-alone drug plan or a Medicare Advantage plan that integrates coverage for medical and drug expenses.
Tag Cloud
Archives
Enter Your Email